Accurate and timely test results are the cornerstone of diagnosis. Successful testing protocols save lives—but when not performed adequately, they can put lives at risk.
Diagnostic errors were the most common allegation in an analysis of 350,000 malpractice claims from the National Practitioner Data Bank. According to the data, diagnostic error represents 29% of claims and 35% of malpractice-insurance payouts. Additionally, 41% of claims involving diagnostic error result in death, compared to 24% of claims involving other allegations. Not only is diagnostic error a frequent cause for patient risk, but it is also deadly.
Testing at the Center of the Diagnostic Process: Steps for a Closed Loop
“Implementation Approaches for Closing the Loop,” a white paper produced by Emergency Care Research Institute (ECRI), defines diagnostic error as “any mistake or failure in the diagnostic process leading to a misdiagnosis, a missed diagnosis, or a delayed diagnosis.” ECRI divides the diagnostic process into eight stages, with testing at the center:
- Access and presentation
- History-taking and collection
- Physical exam
- Testing
- Assessment
- Referral
- Follow-up
- Ongoing monitoring
In some instances, risk can be mitigated by seeking systemic feedback on diagnostic performance and implementing improvement processes based on those outcomes. The phrase “closing the loop” is used to encompass the necessary testing steps, from order through monitored follow-up.
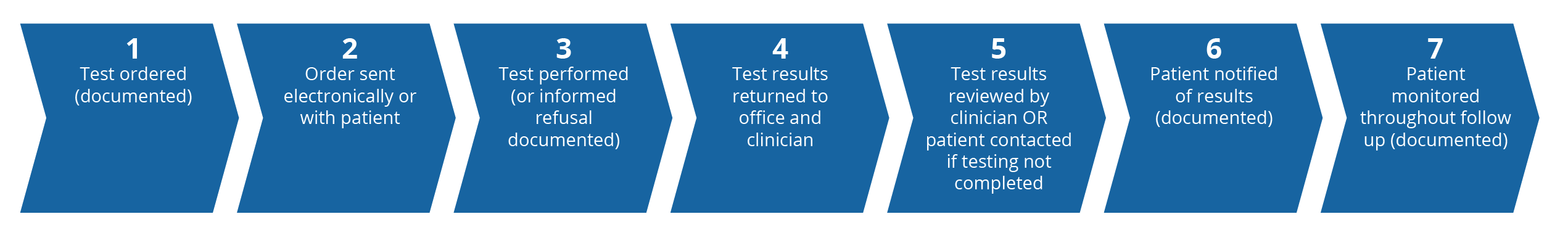
A successfully closed loop on testing includes the following steps:
- Every test has an order documented in the patient record.
- The record contains evidence that the order is sent electronically or in paper form with the patient.
- The ordered test is obtained by the patient in the timeframe ordered; or the patient record contains documentation of the informed-refusal process, if they do not want to undergo testing.
- The result is transmitted to the ordering provider (via interface or through a manual process).
- Results are reviewed in a timely manner by the ordering party or their designee; or when the test is not obtained in the designated timeframe, the patient is contacted to inquire why (and testing is reordered if indicated) and the review/inquiry is documented in the patient record.
- Patient notification of test results is documented in the patient record.
- Continued patient monitoring throughout the follow-up phase (additional testing, prescriptions, specialty referrals, etc.) is documented in the record.
Office Testing Process
How Testing Can Go Wrong
Testing mishaps can be due to systemic issues, human error, patient noncompliance, or all of the above. The following real-life claim examples serve to demonstrate a couple of the many ways testing protocol can go off the rails, at times resulting in catastrophic patient outcomes and potential litigation.
CLAIM: Delayed Diagnosis Due to System Error
An STD screening test resulted as reactive, so the system should have automatically triggered a reflex for the Western blot, but it did not. (A reflex is subsequent testing to the initial test results and is used to further identify significant diagnostic information.) Since it was not flagged as abnormal, nothing within the record indicated to the provider that they should open the results to view that it was reactive. Due to this, the provider instructed the medical assistant to inform the patient that he was negative for HIV. The patient’s health declined over the next six years, and they were admitted to the hospital. A rapid HIV test was administered at the hospital and the patient was found to be positive. The delayed diagnosis in turn delayed treatment options that could have created better quality of life and reduced suffering for the patient during the years prior to diagnosis.
Risk-management advice:
- Confirm that your electronic health record flags results appropriately. Physicians reviewing many lab results per day depend on the system to alert them when something is abnormal or requires additional testing.
- Confirm implementation and provide ongoing monitoring of orders designed to trigger a reflex order if indicated. Are the systems reflexing as designed? Is the reflexed order now showing in the patient record?
- Communicate the right information—including data needed for interpretation—to the right people, at the right time, in the right format. Do not deviate from defined workflows/formats.
CLAIM: Delayed Diagnosis Due to Unintentional Lab Cancellation
A prostate serum antigen (PSA) screening was ordered and cancelled within the same day, due to a non-fasting patient. The patient agreed to return when fasting, but did not. They eventually registered a 3.7 PSA level more than two years later, a level requiring close monitoring. The trend of intermittent patient noncompliance continued, with missed or cancelled tests. However, four years later, a colonoscopy reported a normal rectal exam.
In a follow-up appointment a year after the colonoscopy, the patient was again shown to be noncompliant with lab orders and reported a decrease in urine volume. After a physical exam found a smooth prostate more than three or four inches in size, the doctor ordered free and total PSA checks for the same day. For unknown reasons, the lab cancelled this order. A little less than a year later the patient returned, reporting a variety of symptoms, including urinary urgency and frequency. Their prostate was enlarged and firm, and their PSA was 199.8—well above the normal range. In addition to pursuing a medical-malpractice claim against the physician, plaintiffs also pursued a corporate negligence claim against the clinic entity, related to alleged errors at the clinic’s lab pertaining to PSA tests that were discontinued or canceled.
Risk-management advice:
In the lab:
- Educate lab staff to never cancel a lab order without notifying the ordering provider.
In the physician’s office:
- Provide patients with the information they need to make informed care decisions.
- List the patient’s responsibilities as part of the written plan and provide a copy to the patient.
- Ensure that all written materials provided are in a language that the patient can read.
- Emphasize to patients that they have responsibility for their own health.
- Encourage patients to schedule follow-up appointments prior to leaving, send appointment reminders, etc.
- Request that patients respond to reminder calls and notifications regarding appointments, referrals, diagnostic tests, or medication refills.
- Document with specificity nonadherent or noncompliant behavior in the patient record.
- Discuss and document in the patient record the patient’s understanding of the risks of continued noncompliance.
Conclusion
Missing one or more of the steps in the testing process could lead to adverse medical events and medical-malpractice claims. Closing the loop in testing involves multiple departments, requires working successfully with outside organizations, and could involve patients who are not fully engaged in timely participation of their own care. Whether your facility processes its own tests or relies on another facility, be sure you are in clear communication with all collaborators to always close the loop, and ensure that patients are aware of the impact of noncompliance.
You can avoid some diagnostic error by implementing and monitoring your organization’s defined testing process. Physicians Insurance provides consultative support, plus partners with healthcare organizations like ECRI that create white papers, step-by-step guides, safety recommendations, and implementation strategies for clinicians who want to better use technology and modify their practice to improve information tracking. This support can be used to develop or improve upon your organization’s process.
To reach a risk manager, call (800) 962-1399 or email riskmanagement@phyins.com.
Implementation Approaches for Closing the Loop (ecri.org).
Schiff GD, Hasan O, Kim S, et al. Diagnostic error in medicine: analysis of 583 physician-reported errors. Archives of Internal Medicine. 2009;169(20):1881–1887. [PubMed]
Schiff GD, Puopolo AL, Huben-Kearney A, et al. Primary care closed claims experience of Massachusetts malpractice insurers. JAMA Internal Medicine. 2013;173(22):2063–2068. [PubMed]